Pseudoachalasia Definition, Symptoms, Causes, Treatment, ICD-10 | Achalasia vs Pseudoachalasia
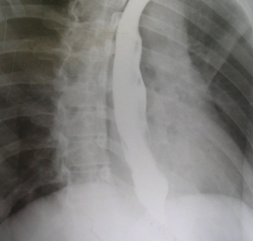
Pseudoachalasia, also known as secondary achalasia, is a constriction of the distal esophagus brought on by a gastroesophageal junction cancer or, in rare cases, a benign condition like Chagas disease. Radiographs of pseudoachalasia look like those of primary achalasia because both conditions can cause a tapered narrowing of the end of the esophagus, dilatation, and aperistalsis (when the esophagus doesn't move).
In spite of the fact that primary achalasia and pseudoachalasia may be indistinguishable from one another, the characteristics of carcinomas of the gastroesophageal region that suggest pseudoachalasia should always be checked out when analyzing barium scans. These include shouldering, eccentricity from mass effect, and nodularity of the distal tapering segment. In pseudoachalasia, the constricted distal section may be long—more than 3.5 cm. The two most frequent cancers associated with pseudoachalasia are adenocarcinomas of the gastric cardia and distal esophagus.
Pseudoachalasia Definition
Pseudoachalasia, also known as secondary achalasia, is a form of achalasia-pattern esophageal dilatation that occurs when the distal esophagus becomes constricted for reasons other than original denervation. Malignancy, specifically submucosal gastric cancer, is one of the most common causes, and it frequently spreads into the lower esophagus as well.
Pseudoachalasia Symptoms
Patients who have pseudoachalasia frequently experience growing dysphagia, chest discomfort, regurgitation, and weight loss. Patients also often report having difficulty swallowing. When viewed by radiography, the esophagus is typically enlarged and aperistaltic, with a gradually narrowing distal end. Esophageal manometry reveals signs of aperistalsis, increased pressure in the LES, and inadequate relaxation of the LES in response to deglutition. Patients who have pseudoachalasia are frequently given an initial diagnosis of achalasia, which can result in unnecessary dilations of the esophagus. Adenocarcinoma which originates in the gastric fundus is the most frequent causal lesion of pseudoachalasia.
Pseudoachalasia Causes
Pseudoachalasia has been established as a separate pathophysiologic entity due to the numerous case reports that have been published on the topic. Patients who have pseudoachalasia frequently experience growing dysphagia, chest discomfort, regurgitation, and weight loss. Patients also often report having difficulty swallowing. The esophagus is often radiographically dilated, aperistaltic, and smooth tapering toward its distal end. Esophageal manometry reveals signs of aperistalsis, increased pressure in the LES, and inadequate relaxation of the LES in response to deglutition. Patients who have pseudoachalasia frequently receive an initial diagnosis of achalasia, which raises the possibility of unnecessary dilations being performed on these patients. Adenocarcinoma with gastric fundus origin is the most frequent causal lesion for pseudoachalasia. Furthermore, metastases from cancers of the lung, prostate, hepatic region, pancreatic region, and lymphoma have all been documented to generate what is variously referred to as secondary achalasia or pseudoachalasia.
Pseudoachalasia Treatment
Achalasia is a degenerative neurological lesion that cannot be healed. As a result, the focus of treatment is on symptom relief and avoiding consequences. Since peristalsis almost never returns after receiving treatment, this is mostly achieved by lowering LES pressure. Three treatment options are available to lower LES pressure: medication, a powerful pneumatic dilatation, and surgical myotomy.
These treatments aim to improve gravity esophageal emptying by reducing sphincter tone while maintaining an appropriate barrier against gastroesophageal reflux in order to reduce obstructive LES pressure. In the majority of patients, regurgitation is reduced, and swallowing can return to almost normal quality. In most cases, symptom relief follows improvement and stabilization of esophageal emptying in the standing posture, which may indicate long-term success.
Achalasia vs Pseudoachalasia
Pseudoachalasia, also known as secondary achalasia, is a rare form of esophageal dysmotility syndrome that presents with symptoms and manometric results that are indistinguishable from those of primary achalasia.
Both achalasia and pseudoachalasia are associated with a similar symptom known as the thickening of the esophageal wall. Patients with pseudoachalasia were seen to have asymmetrical esophageal wall thickening that was greater than 10 millimeters, particularly at the gastroesophageal junction (GEJ). The same study indicated that symmetrical esophageal wall thickening that was less than 10 millimeters was likely to be achalasia.
Pseudoachalasia ICD-10
For the purpose of payment, the ICD-10-CM code K22.0 can be used to identify the diagnosis of achalasia of the cardia. ICD-10 code K20 through K31 especially refers to conditions affecting the esophagus, stomach, and duodenum.
 Reviewed by Simon Albert
on
October 25, 2022
Rating:
Reviewed by Simon Albert
on
October 25, 2022
Rating:











